Abstract
Impedance
plethysmography (IPG) is a safe, noninvasive method for measuring peripheral hemodynamics.
The purpose of is to describe the IPG technique and its potential use by
physical therapists in making hemodynamic evaluations. Impedance plethysmography
requires the attachment of four circumferential Mylar band electrodes around a
limb. We use a cardiograph to introduce a 4-mA current (I) at a frequency of
100 kHz in the two outer electrodes. The voltage (V) is sensed in the two
center electrodes, and the resulting impedance (Z) is calculated using Ohm's
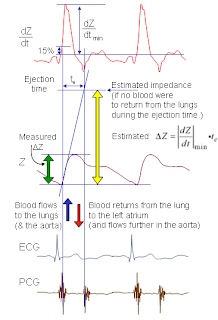
law (Z = V/l) as shown in (Figure 1) . Arterial blood flow can be
calculated using an impedance-related volume conduction equation. Impedance
plethysmography has been shown to be economical, and any limb or limb segment
can be evaluated. Applications are presented for the assessment of arterial
blood flow, peripheral arterial disease, deep vein thrombosis, and venous
insufficiency. Impedance plethysmography offers the physical therapist a safe
and relatively simple technique to assess the peripheral vascular status of the
patient.
Background
Plethymography is a non-invasive diagnostic treatment used for screening
and patient follow-ups with various arterial and venous pathologies.
This treatment is concerned with the measurement of volume and volume
displacement of blood. The screening provides a circulatory assessment via a
waveform representation of pulsatile peripheral blood flow. Instrumentation
providing blood volume parameters exists but nothing to measure volume
directly.
An example of this instrumentation is the use of an ultrasound. While
ultrasound provides hemodynamic (hemodynamic refers to the forces generated by
the heart and the motion of blood through the cardiovascular system) data on
vein segments, plethysmography provides information that is indirectly related
to venous volume changes. The data obtained is not specific to venous function
because limb volume changes may be caused by several factors.
Figure 1. Impedance
plethysmography.
Plethysmograph Components
The main part of a very simple plethysmograph (Figure 2)
is a container of suitable size and shape in which the part, for example, hand,
leg, or finger, is placed. In animal experiments a kidney, heart, or spleen may
be studied. The container is filled with water and hermetically sealed. (In
Figure 2 a rubber cuff is used.)
Changes in the water level in the container reflect
fluctuations in blood volume in the organ or part and are recorded in the form
of a curve called a plethysmogram. The plethysmogram shows small fluctuations
in blood pressure corresponding to pulse and somewhat larger ones corresponding
to respiration; large variations reflect vascular reactions to various stimuli.
More advanced methods of plethysmography include (1) photoplethysmography, in
which light is directed through an organ, such as an ear or finger, onto a
photoelectric cell, or light is reflected from the organ, (2)
rheoplethysmography, and (3) dielectrography, or rheocardiography. The last two
methods are based on the direct recording of fluctuations in the electrical
properties of an organ, which reflect the dynamics of the organ’s blood supply.
Figure 2. Plethysmograph Components.
Plethysmography procedures
Rapid changes are typically associated with changes in blood volume or
movement artifact. If movement is controlled, information specific to blood
volume can be obtained. Further separation of arterial and venous flow effects
can be observed through electronic filtration. Venous flow changes typically
involve long transient time constants with duration of seconds or minutes.
Venous displacement measurements are typically associated with shifts in
body position and limb compressions which allow measurements of magnitude and
duration. Four main types of plethysmography exist. They include
Air-Displacement, Photoelectric, Strain gauge, and Impedance. Air-Displacement
plethysmography (Figure 3) deals with measuring the volume of an object
by indirectly measuring the volume of air it displaces inside a closed chamber.
The human body volume is measured when a patient sits in an enclosed chamber
and displaces a volume of air equal to his or her own body volume.
Figure 3. Air Displacement Plethysmography.
By subtracting the remaining volume of air inside the chamber when the
patient is inside from the volume of air in the chamber empty, you get the body
volume. Photoelectric plethysmography is concerned with assessment based on
cutaneous blood volume. An electrode consisting of an infrared LED and a
photosensor is attached to the skin. Light transmitted into the skin is
scattered and absorbed by tissue in the illuminated field. Blood attenuates the
reflected light and intensity of reflected light changes with blood tissue
density. The voltage signal generated by the photosensor is amplified by a DC
circuit. Low frequencies are passed which produces relatively stable tracing.
This corresponds to blood density in the underlying tissue. Strain gauge
plethysmography uses a transducer filled with mercury or indiumgallium metal
alloy conductor.
Stretching the strain gauge causes a decrease is diameter causing an
increase in voltage. When wrapped around a limb segment, the gauge provides a
circumferential measurement that can be used to compute area. The “slice
volume” of the limb segment changes as the limb volume expands and contracts.
The final type of plethysmography is impedance plethysmography. A weak current
is passed through a limb and the electrical resistance to current flow is
measured. Four conductive bands are taped around the limb as outer and inner
pairs of electrodes. The inner pair is then used to measure electrical
resistance.
Photo Sensor Plethysmography Design & Work Procedures as a type of Plethysmography kinds
The finger is
placed into a box with a red LED on one side and a Cadmium Sulfide (CdS) cell
on the other side (Figure 4). The resistance of the CdS cell varies with
the intensity of the light hitting it, and this intensity depends on the amount
of blood in the finger.
The change in
the resistance is transduced into a change in voltage, and in its raw form
gives a voltage range of 0 to 2.5 volts. We want to measure the variation in
this signal caused
by the pulsatility of blood flow in the finger. By carefully examining the raw
signal on an oscilloscope, we found that this variation is at most 10mV. This
signal must be amplified into a 0-5 V range to take advantage of the full range
of the A/D converter.
The raw signal
also includes a
great deal of noise which must be filtered out. After being converted to
digital, the signal is analyzed using the PIC microcontroller, and the output
is displayed on a 10-LED ladder. In one mode, the LEDs are set up to all light
up when the CdS detects little light from having most of it blocked by the
blood flow, and all turn off when encountering much light, corresponding to no
fluid. In the second mode, the heart rate in beats per minute (bpm) is
calculated from the period of the signal and different LEDs are lighted to
indicate the bpm range in which the heart rate falls.
Figure
4.
Transduction, Amplification, and Filtration
Single supply design (Vcc = 5V) was required to power the circuit
components.
TRANDUCTION
The CdS cell changes resistance in response to the amount of light
it receives. To work with this signal requires that it be transduced into
a voltage. The CdS cell was placed in series with a 47 kOhm resistor, and the
signal was taken between them. The signal then ranged from 0 to Vcc/2 or 2.5
volts as the CdS resistance varied.
AMPLIFICATION
We chose the inverting configuration of an amplifier (Figure 5) as it is
common to use this kind in single supply design. These amplifiers can output
voltages quite near the power supply voltage. And since we wanted to measure
the changes of the 2.5 voltage signal due to the blood flow, we needed to
amplify the changes rather than the entire signal. We also needed the signal in
the 0-5V range after amplification, rather than being centered around 0V. A
virtual ground was employed to achieve this by amplifying the changes with
respect to the Vcc/2 volts. amplifier was used and attached to the positive
terminal of the op-amp to function as a virtual ground. Below is a diagram of
the design constructed so far.
Figure 5. Amplification By Invering Amplifier.
Notice that the inverting configuration was chosen because it can
easily be modified to also act as a filter as we shall soon see. A secondary
gain stage was implemented using the same configuration to invert the inverted
signal from the primary gain stage.
The gain of an inverting amplifier is equal to -Rf/Ri where Rf is
the feedback resistance and Ri is the input resistance. Because the gain stages
will function with the filtering, we will consider the gain in the next
section.
FILTRATION
Once again, the signal we want to end up with consisted of tiny
variations (changes in light intensity due to blood flow into and out of the
finger), superimposed on a large constant signal (average light flowing through
finger). Recall that we only want the time varying part of the signal
amplified, and if we were to amplify the raw signal, the DC (constant) part of
the signal would saturate the amplifier before obtaining desired amplification
of the AC (time varying) part.
To get rid of the DC signal we used a high-pass filter (Figure
6) because DC signals are extremely low frequency. We had to be careful,
however, not to attenuate the pulse signal, which is usually about 1 Hz
(equivalent to one heart beat per second). High frequency noise was a concern
as well with most of it coming from the 120 Hz signal of the light fixture (due
to positive and negative portions of the 60 Hz power noise). Considering these
requirements, a band-pass filter with a frequency band from .5 Hertz to 10
Hertz was chosen. We decided that a second-order simple band-pass filter, which
could be implemented by modifying the amplifier design, would be sufficient. A
capacitor in series with the input resistance constitutes a high-pass filter,
and one in parallel with the feedback resistance constitutes a low-pass. RC
values were selectively chosen to set not only the pass-band frequencies, but
also the gains.
Figure
6. High Pass Filter.
DISPLAYING
THE PULSE AND MEASURING THE HEART RATE
To
measure the amoung of blood flow in the finger as well as the time between each
beat on a 10-LED ladder. The algorithms to perform this task upon a push of a
button are explained below.
To
display the blood flow measured by the photoplethysmograph we used a ladder of
ten LEDs, with the number of lit LEDs increasing as the amount of the blood in
the finger increased. This was done by setting a threshold for each
LED--the higher the LED on the bar, the higher the threshold and vice versa. When
the digital signal went above the threshold for a given LED, the PIC
microcontroller would output a logic high, thus lighting the LED. In
order to have enough outputs from the PIC to control all the LEDs in the bar,
we could only have one input into the PIC.
In
addition to showing the signal using the LEDs, we also wished to display
information about heart rate. We did this by lighting 5 LEDs (every other
bar on the ladder) to indicate a heart rate above an appropriate threshold
(> 40bpm, > 50bpm, etc.). The circuit's mode of operation (heart
rate or pulse) was controlled by a push button on the printed circuit board
containing the microcontroller. We used a state machine (see diagram
below) to control the process of calculating the number of heart beats per
minute (bpm). First, we found the minimum and maximum value of the signal
over a 3 second interval, then we chose a low threshold at the minimum value
plus a quarter of the range and a high threshold at the maximum value minus a
quarter of the range. We started a counter when the signal passed the
high threshold from below and stopped the counter when the signal passed the
high threshold again after having passed the low threshold. The heart
rate, in beats per minute, was then calculated from this period. The
displayed heart rate was a weighted average of the current calculation and the
previous two (a [1 1 2] filter) (Figure 7).
Figure 7.
oscilloscope
printouts of the raw signal after the signal processing (Figure 8)
Figure 8.